Table of Contents
ToggleIntroduction
The human immune system is a complex network of specialized cells, tissues, and organs designed to protect the body against infections, cancer, and foreign invaders. At the heart of this system are the immune cells—each with a unique function in detecting, responding to, and remembering pathogens.
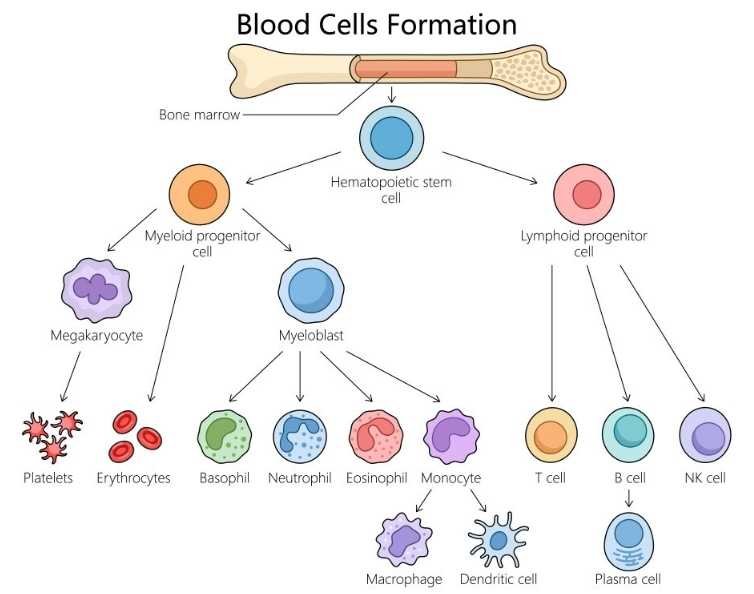
These vital defenders originate from a common source: hematopoietic stem cells in the bone marrow.
In this article, we explore the different immune system cells, their origin, structure, and crucial roles in innate and adaptive immunity.
Hematopoietic Stem Cells: The Origin of Immunity
- Hematopoietic (blood-forming) stem cells are self-renewing, pluripotent cells that can develop and differentiate into various immune system cell types.
- They are in charge of continuously regenerating blood, which involves producing billions of new blood cells daily.
- The most crucial cell in bone marrow transplants is the hematopoietic stem cell, which has the capacity to produce the whole immune system.
- These stem cells are central to bone marrow transplants, which aim to restore immunity and blood cell production in patients with leukemia, lymphoma, and other hematologic disorders.
- The hematopoietic stem cell differentiates into either a common myeloid progenitor cell or a common lymphoid progenitor cell along one of two routes. They all further differentiate into other cell kinds.
- HSCs follow two primary differentiation pathways:
- Common Myeloid Progenitor (CMP) cells
- Common Lymphoid Progenitor (CLP) cells
- Each pathway leads to the development of specific immune and blood cell types, regulated by local growth factors and cytokines in the bone marrow niche.
Myeloid Progenitor Cells: Innate Immunity’s First Responders
Myeloid Progenitor cells are dedicated to a specific cell lineage and have forfeited their ability to self-renew. Myeloid stem cells give rise to progenitors of platelets and red blood cells, as well as white blood cells (neutrophils, eosinophils, basophils, monocytes, mast cells, and dendritic cells).
Progenitor cells multiply and develop into relevant cell kinds in the presence of suitable factors and cytokines.
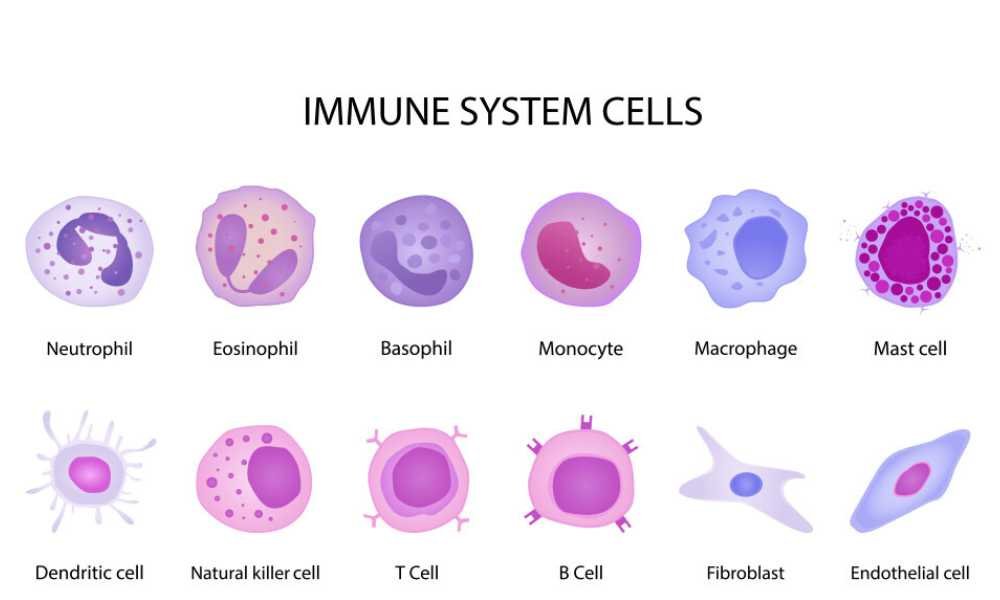
Neutrophils
- Neutrophils are polymorphonuclear (PMN) leucocytes with a multilobed nucleus and granules in the cytoplasm. They make up 50 to 70 percent of all circulating white blood cells, have a lifespan of 34 days, and spend 78 hours in the blood before migrating to tissues.
- Neutrophils are also known as polymorphonuclear leukocytes.
- Neutrophils engulf pathogens via phagocytosis, produce antimicrobial substances, and form neutrophil extracellular traps (NETs) to capture and destroy microbes.
- They are stained with both acidic and basic dyes.
- The diameter of neutrophils is 1114 μm.
Monocytes
Monocytes, which are similar to neutrophils, circulate in the blood. They account for 510% of the total white blood cells. Additionally, they cover the interior surfaces of blood vessels in organs such as the spleen and liver. Here, they take microorganisms in the blood as they pass by. Monocytes transform into macrophages when they exit the circulation and infiltrate the tissues, changing in both size and form.
Macrophages
Macrophages are immune, mononuclear cells that originate from the myeloid progenitors of the hematopoietic system. They participate in the identification, phagocytosis, and elimination of pathogens.Macrophages are referred to as microglial cells, kupffer cells, alveolar macrophages, and osteoclasts, among other names, depending on the tissue they are in.
Dendritic Cells
The most crucial antigen-presenting cells (APCs) for stimulating naïve T cells are dendritic cells. They possess phagocytic abilities and lengthy membranous extensions. Dendritic cells are crucial in connecting innate and adaptive immune responses, as well as in innate reactions to infections. They present microbial antigens to T lymphocytes.
Basophils
Basophils are blood granulocytes (these granules bind with basic dyes) that have a lot in common with mast cells in terms of their structure and function. They make up less than 1% of blood leukocytes and originate from bone marrow precursors. Basophils are not typically found in tissues, but they can be recruited during certain inflammatory responses. Antigen binding to IgE can induce basophils because they produce receptors for IgG and IgE and bind IgE.
Eosinophils
These are blood granulocytes that have cytoplasmic granules with enzymes that can damage the cell walls of parasites. Eosinophils are in charge of controlling inflammatory reactions and taking part in immediate allergic reactions. Acidic dyes like eosin bind to the basic proteins found in eosinophil granules. Normally, eosinophils can be found in peripheral tissues, particularly the mucosal linings of the respiratory, gastrointestinal, and genitourinary systems.
Red Blood Cells (RBCs)
- Red blood cells, also called erythrocytes, are the most common cells in the blood and are mostly in charge of delivering oxygen from the lungs to the tissues of the body and transporting carbon dioxide back to the lungs for exhalation.
- They have haemoglobin, a red pigment that binds oxygen effectively.
- The unique biconcave shape of red blood cells enhances their surface area for gas exchange and enables them to pass through tiny blood arteries.
- Mature RBCs have no nucleus, unlike the majority of other cells, which allows for more haemoglobin.
- They are created in the bone marrow and, before being broken down in the spleen and liver, last for around 120 days.
White Blood Cells (WBCs)
- Leukocytes, sometimes referred to as white blood cells, are a vital part of the immune system and aid the body in warding off infections, outside intruders, and aberrant cells.
- WBCs are fewer in number and bigger in size than red blood cells, and they also contain a nucleus.
- They fall into several categories, such neutrophils, eosinophils, basophils, monocytes, and lymphocytes, each of which has a distinct function in the body’s defenses against infection, inflammation, and allergies.
- Depending on the kind, WBCs can live for a few hours or for many years.
- They are made in the bone marrow and lymphatic tissue.
- They are always on the lookout for signs of infection or harm as they circulate throughout the blood and tissues.
Lymphoid Progenitor Cells: Architects of Adaptive Immunity
- Common lymphoid progenitor cells produce some dendritic cells as well as B, T, and NK (natural killer) cells.
- The primary cells of the immune system are lymphocytes, which are in charge of immunological memory and adaptive immunity.
- Diversity, self/non-self-recognition, and specificity are other key features of lymphocytes.
- 99% of the cells in the lymph are lymphocytes, which make up 20–40% of the body’s white blood cells. We have around 10^11 lymphocytes in our body.
- When they receive signals, these lymphocytes continuously circulate in our blood and lymph and move to infection sites.
B Lymphocytes (B Cells)
- B lymphocytes, sometimes referred to as B cells, are specialized immune system cells whose primary role is the production of antibodies, also known as immunoglobulin.
- The letter designation for B lymphocytes originated from the location of their maturation, the bursa of Fabricius in birds. In the bone marrow, where they also undergo immunological training and maturation, hematopoietic stem cells give rise to B cells.
- When B cells come into contact with foreign antigens, they react by turning into plasma cells, which are antibody-secreting cells.
- Additionally, B cells can develop into memory cells, which mediate a faster and stronger secondary immune response.
T Lymphocytes (T Cells)
- T cells, also known as T lymphocytes, originate in the bone marrow from hematopoietic stem cells but finish their maturation in the thymus (the “T” stands for thymus).
- Similar to B lymphocytes, these cells contain membrane receptors for antigens called T cell receptors (TCR).
- T cells target virus-infected cells and also serve as regulators of the immune system.
- Based on their functions, T cells may be divided into three main categories:
- Cytotoxic, or “killer,” T cells (CD8 T cells): Kills virally infected or changed self-cells.
- Helper T cells (CD4 T cells) stimulate B cells.
- Regulatory T cells assist in reducing the immune response
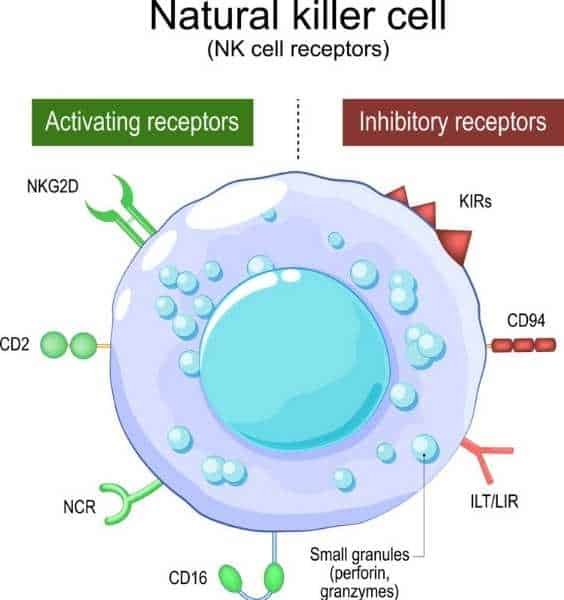
Natural Killer (NK) Cells
- Natural killer (NK) cells are large granular lymphocytes that recognize and eliminate virus-infected and tumor cells without prior sensitization.
- Because they can easily kill cells infected with viruses without the need for thymus training (which T cells need), natural killer (NK) cells are given their name.
- NK cells are able to kill both virally infected cells and aberrant self-cells (cancer cells).
- The bloodstream and tissues contain a comparatively small number of NK cells. They are big, granular lymphocytes that lack the surface markers characteristic of B or T cells.
Key Characteristics of Immune Cells
| Immune Cell | Origin | Main Function | Part of Immunity |
| Neutrophils | Myeloid | Phagocytosis, NET formation | Innate |
| Monocytes/Macrophages | Myeloid | Phagocytosis, antigen presentation | Innate |
| Dendritic Cells | Myeloid/Lymphoid | Antigen presentation | Bridge (Innate/Adaptive) |
| Basophils | Myeloid | Allergy, parasite defense | Innate |
| Eosinophils | Myeloid | Parasite killing, allergy | Innate |
| B Cells | Lymphoid | Antibody production | Adaptive |
| T Cells | Lymphoid | Cell-mediated immunity | Adaptive |
| NK Cells | Lymphoid | Virus and tumor killing | Innate-like |
Conclusion: A Unified Immune Defense Network
The immune system is an intricate cellular network originating from hematopoietic stem cells. These stem cells differentiate into either myeloid or lymphoid progenitors, creating an army of specialized cells that defend against pathogens, clear debris, and maintain homeostasis.
- Innate immune cells— Including neutrophils, macrophages, dendritic cells, eosinophils, and basophils—act as first responders.
- Adaptive immune cells— B cells, T cells, and NK cells—provide targeted and long-lasting immunity.
Understanding the development and function of these cells has profound implications for immunotherapy, vaccine development, autoimmune disease management, and transplant medicine.
As research continues to uncover the complexities of immune cell interactions, we gain new tools to combat disease and enhance health.
Frequently Asked Questions (FAQs)
Q1: What is the primary difference between innate and adaptive immune cells?
Innate immune cells offer immediate, non-specific defense, while adaptive immune cells respond more slowly but provide highly specific and long-lasting protection.
Q2: Which immune cells are responsible for memory in the immune system?
Memory B cells and memory T cells retain information about past infections and respond more efficiently during subsequent exposures.
Q3: Why are hematopoietic stem cells important in bone marrow transplants?
They can regenerate the entire blood and immune cell population, making them essential for patients with immune or hematological disorders.
Also Read
- Biochar: Properties, Production, and Applications
- Ribonucleic acid (RNA): Types, Structure & their Function
- Antimicrobial Resistance (AMR) Mechanisms and Alternatives
- Microscopy: Principles, Types, and Applications
- Microbiology: From Microorganisms to Career Opportunities
- Spirulina: The Superfood Microalga with Limitless Potential
- Bacteriology Quiz
- Medical Microbiology Quiz
- Basic Microbiology Quiz

