Table of Contents
ToggleIntroduction
Antimicrobial Susceptibility Testing (AST) is a fundamental laboratory procedure in clinical microbiology used to determine how effectively antimicrobial agents, such as antibiotics, inhibit or kill bacteria. The main objective of AST is to evaluate whether a microorganism is susceptible, intermediate, or resistant to various antimicrobial drugs.
With the rise of antimicrobial resistance (AMR), AST plays a crucial role in guiding healthcare professionals to choose the most effective antibiotic, optimize dosage and duration, and avoid unnecessary drug use. This leads to better patient outcomes, reduced treatment failures, and helps combat the global threat of antibiotic resistance.
Principle of Antimicrobial Susceptibility Testing
The principle of AST is based on evaluating the ability of antimicrobial compounds to inhibit the growth of microorganisms under controlled laboratory conditions.
The process involves:
- Isolation and identification of the pathogenic microorganism from a clinical sample.
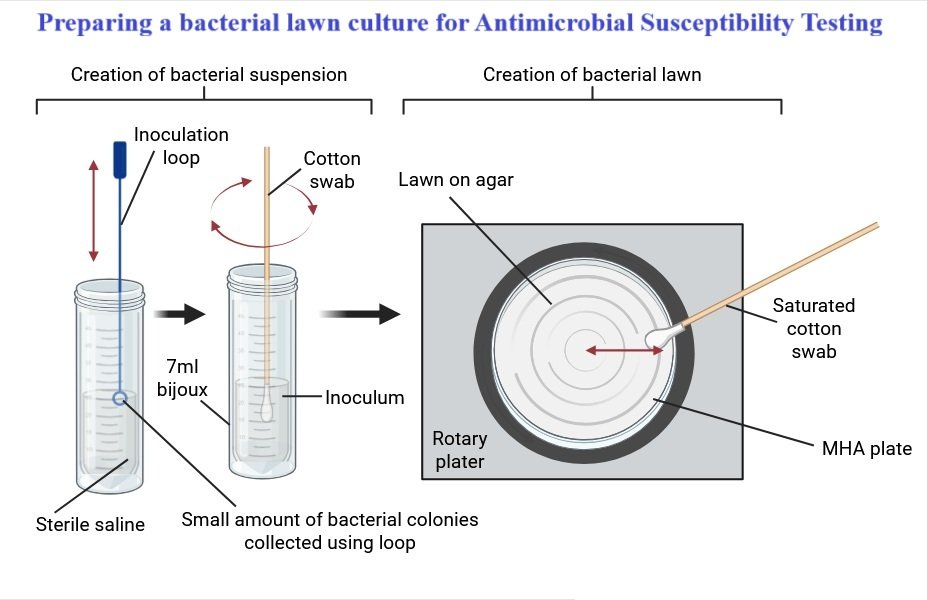
- Preparation of a standardized inoculum that ensures consistent microbial concentration.
- Exposure of the microorganism to specific antimicrobial agents using standardized techniques such as the disk diffusion or broth dilution method.
- Measurement of inhibition (zones or MIC) to determine susceptibility or resistance.
The Minimum Inhibitory Concentration (MIC) is the lowest concentration of a drug that prevents visible growth of a microorganism. MIC values are interpreted using standard reference guidelines such as CLSI (Clinical and Laboratory Standards Institute) or EUCAST (European Committee on Antimicrobial Susceptibility Testing).
Test Methods in AST
Different techniques are used to determine the antimicrobial susceptibility of microorganisms. The most widely used methods include:
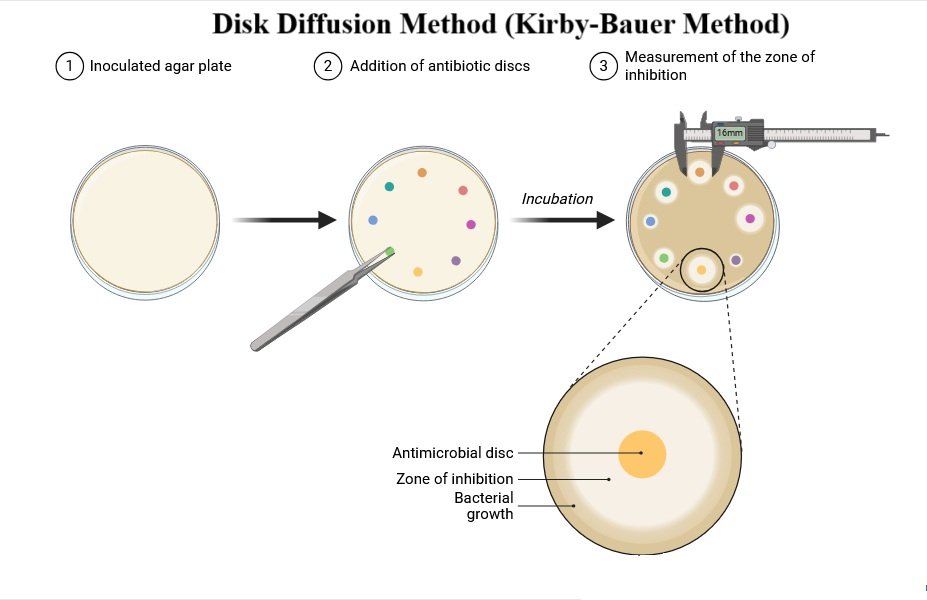
1. Disk Diffusion Method (Kirby-Bauer Method)
This is the most common and standardized technique for antimicrobial susceptibility testing.
Principle:
The method depends on the diffusion of antimicrobial agents from paper disks into the agar medium, where they inhibit bacterial growth.
Procedure:
- A standardized bacterial suspension is uniformly spread over the surface of Mueller-Hinton agar.
- Paper disks impregnated with known concentrations of antibiotics are placed on the agar surface using sterile forceps or a disk dispenser.
- Plates are incubated at 35–37°C for 16–18 hours.
- After incubation, the zones of inhibition around each disk are measured in millimeters using a ruler or caliper.
- Zone sizes are compared with CLSI or EUCAST interpretive charts to classify the bacteria as susceptible (S), intermediate (I), or resistant (R).
2. Broth Dilution Method
This method is used to determine the Minimum Inhibitory Concentration (MIC) of an antimicrobial agent.
Principle:
Microorganisms are exposed to a range of antibiotic concentrations in liquid broth to identify the lowest concentration that inhibits visible growth.
Procedure:
- Serial dilutions of the antimicrobial agent are prepared in a liquid medium.
- A standardized inoculum of the microorganism is added to each dilution.
- Tubes or wells are incubated for 18–24 hours.
- After incubation, the tubes are examined for turbidity or microbial growth.
- The MIC is the lowest concentration that shows no visible growth.
Step-by-Step Procedure for Antimicrobial Susceptibility Testing
- Isolation and Identification of the Microorganism: The microorganism is isolated and identified by using the appropriate laboratory methods to get a pure culture from the clinical sample. Using biochemical tests or molecular techniques, determine the species of the microbe.
- Preparation of a Standardized Inoculum: Prepare the microorganism’s uniform inoculum. Using a particular McFarland standard, which gives a turbidity equivalent to a certain concentration of microbial cells, regulate the inoculum’s density.
- Inoculation of Culture Media: Introduce the regulated inoculum onto the proper culture medium. Mueller-Hinton agar is frequently employed for bacteria, whereas Sabouraud agar is used for fungi. Using a sterile loop or swab, streak the agar surface or distribute the inoculum uniformly.
- Application of Antimicrobial Disks or Dilution Setup:
- Disk Diffusion Method (Kirby-Bauer Method):
- Put sterile paper discs treated with particular concentrations of antimicrobial chemicals on the agar surface.
- Gently press the discs to make sure they are in close contact with the agar.
- Use forceps or a disk dispenser to position the disks in a consistent manner, keeping the right spacing between them.
- Broth Dilution Method:
- In a liquid broth, make a variety of concentrations of the antimicrobial agent.
- Make sure the right drug concentrations are reached by adding the standardized inoculum to each broth tube.
- Include tubes with positive growth and negative control that don’t contain any antimicrobials.
- Disk Diffusion Method (Kirby-Bauer Method):
- Incubation: Incubate the culture plates or broth cultures at the ideal temperature for the development of the microbe. The temperature and length of incubation can change depending on the testing technique and the microbe being tested. Maintaining correct temperature and humidity control throughout incubation is essential.
- Measurement and Interpretation:
- Disk Diffusion Method (Kirby-Bauer Method):
- Measure the diameter of the zones of inhibition surrounding each disk after incubation.
- For precise measurements, use a calibrated measuring instrument or a ruler.
- Compare the zone sizes to ascertain whether the organism is vulnerable or resistant to the antimicrobial substances.
- Broth Dilution Method:
- After incubation, check the broth tubes for any signs of growth.
- The MIC is defined as the lowest concentration of a substance that prevents observable development.
- Compare the MIC values with interpretive criteria to assess whether the microbe is susceptible or resistant.
- Disk Diffusion Method (Kirby-Bauer Method):
Interpretation of Results
| Category | Meaning | Implication |
| Susceptible (S) | Microorganism inhibited at achievable drug concentrations. | Antibiotic likely effective in treatment. |
| Intermediate (I) | Partial inhibition at higher drug concentrations. | May be effective at increased doses or specific sites. |
| Resistant (R) | Microorganism not inhibited at achievable drug concentrations. | Antibiotic likely ineffective. |
Applications of Antimicrobial Susceptibility Testing
AST is applied across multiple healthcare and research settings:
- In a hospital environment, antibiotic sensitivity tests can be employed to aid in the treatment of patients with serious or life-threatening infections like sepsis or pneumonia.
- Outpatient environments: Antibiotic susceptibility tests may be used in outpatient settings, such as urgent care centers or primary care clinics, to help direct care for patients with less serious illnesses, such as bronchitis or urinary tract infections.
- Long-term care institutions: Antibiotic sensitivity tests are sometimes utilized in nursing homes and other long-term care facilities to help direct therapy for patients with persistent infections, such as those with weakened immune systems.
- Research environments: Antibiotic sensitivity tests are used in research environments to evaluate how well various antibiotics work against particular bacterial strains or to look at how antibiotic resistance is developing in different communities.
Limitations of AST
While AST provides valuable clinical data, it has some limitations:
- In vivo variability: Laboratory results may not always reflect the actual drug performance in the human body.
- Time-consuming: Especially for slow-growing or fastidious organisms.
- Requires pure cultures: Mixed infections can affect accuracy.
- Standardization challenges: Some pathogens lack established reference values.
- Resistance mechanism detection: Specialized tests (e.g., PCR, molecular assays) are needed to identify specific resistance genes.
- Human or technical errors: Inoculum density, incubation, or interpretation mistakes can lead to inconsistent results.
Conclusion
Antimicrobial Susceptibility Testing (AST) is an indispensable tool in modern microbiology and clinical medicine. It ensures that antibiotic therapy is evidence-based, helping clinicians make data-driven decisions for optimal patient care.
Moreover, AST plays a pivotal role in antimicrobial stewardship by reducing misuse, preventing resistance, and guiding the development of new therapeutic strategies. As the threat of antimicrobial resistance continues to grow globally, effective use of AST remains vital for safeguarding the future of infectious disease treatment.
Frequently Asked Questions (FAQs)
Q1. What is the main purpose of Antimicrobial Susceptibility Testing (AST)?
The main purpose of AST is to determine whether bacteria are susceptible, intermediate, or resistant to specific antibiotics, guiding effective treatment decisions.
Q2. What is the difference between Disk Diffusion and Broth Dilution methods?
The Disk Diffusion Method measures the zone of inhibition around antibiotic disks, while the Broth Dilution Method determines the Minimum Inhibitory Concentration (MIC) of antibiotics in liquid medium.
Q3. What is MIC in antimicrobial testing?
MIC stands for Minimum Inhibitory Concentration, the lowest concentration of an antimicrobial agent that prevents visible bacterial growth.
Q4. Which media is used for the Kirby-Bauer test?
Mueller-Hinton agar is the standard medium used for bacterial susceptibility testing.
Q5. Why is the McFarland standard important?
The McFarland standard ensures a uniform bacterial inoculum, preventing inaccurate results due to variations in bacterial concentration.
Q6. What are the limitations of AST?
AST results may not always correlate with real patient outcomes due to host factors, resistance mechanisms, or laboratory errors.
Also Read
- Plasmids: Structure, Types, Replication, and Applications
- Microbiology of Fermented Foods
- How Microbiology Helps in Vaccine Development: A Comprehensive Guide
- Homogenizer: Principle, Types, Parts, and Applications
- Nitrogen Fixation and Its Importance in the Ecosystem
- Parasitology: An Overview of Parasites, Diseases, and Host Interactions
- Molecular Blotting: Techniques, Uses, and Significance
- Antimicrobial Resistance (AMR) Mechanisms and Alternatives
- Ribonucleic acid (RNA): Types, Structure & their Function
- Microbiology Notes
- Bacteriology Quiz
- Latest Research Topics in Microbiology

