Table of Contents
ToggleIntroduction
Antibiotics are chemical compounds designed to fight bacterial infections. Unlike antiviral medications (which target viruses) or antifungal drugs (which treat fungal infections), antibiotics specifically act against bacteria—unicellular organisms that can reproduce on their own.
Depending on their mechanism of action, antibiotics can either:
- Kill bacteria outright (bactericidal), or
- Inhibit bacterial growth and reproduction (bacteriostatic).
Antibiotics can be:
- Natural – produced by bacteria or fungi to compete with other microbes.
- Semisynthetic – modified from natural compounds to improve stability or activity.
- Synthetic – completely manufactured in laboratories.
The key advantage of antibiotics is that they exploit biological differences between bacterial and human cells, allowing them to eliminate infections without severely harming the host—although side effects sometimes occur.
History of Antibiotics
The story of antibiotics begins with an accident. In 1928, Scottish bacteriologist Alexander Fleming observed that a mold contaminant, later identified as Penicillium notatum, inhibited the growth of Staphylococcus bacteria in his petri dish. He named the active substance penicillin.
However, Fleming’s discovery remained a laboratory curiosity until the 1940s, when Howard Florey, Ernst Chain, and Norman Heatley developed methods for mass production. During World War II, penicillin became a miracle cure, saving thousands of soldiers from infections that once killed more soldiers than bullets.
This success triggered the “Golden Age of Antibiotics” (1940s–1960s), during which scientists discovered many new antibiotic classes, including:
- Streptomycin – the first drug effective against tuberculosis.
- Tetracyclines – broad-spectrum antibiotics.
- Erythromycin – a macrolide alternative for penicillin-allergic patients.
By the 1970s, antibiotics had become an integral part of modern medicine.
Mechanism of Action of Antibiotics
Antibiotics work by targeting specific bacterial structures or metabolic pathways.
Below are the main categories:
- Inhibitors of Cell Wall Synthesis
- Disruptors of the Cell Membrane
- Protein Synthesis Inhibitors
- Inhibitors of Nucleic Acid Synthesis
- Folate Pathway Inhibitors (Antimetabolites)
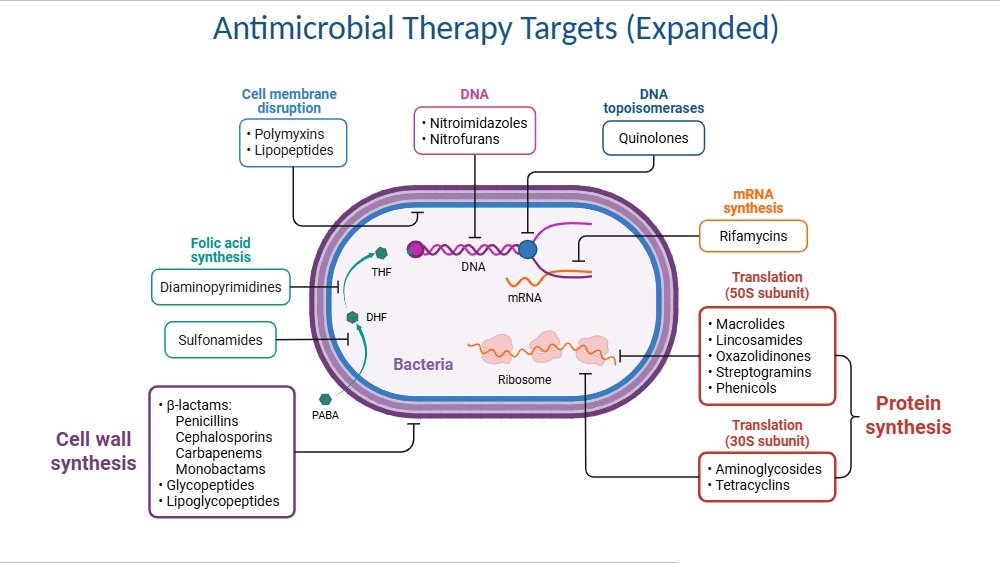
1. Inhibitors of Cell Wall Synthesis
Method: By blocking crosslinking or precursor transport, these antibiotics kill bacteria and disrupt the synthesis of the bacterial peptidoglycan cell wall, resulting in cell lysis.
Examples:
- Beta-lactams → penicillins, cephalosporins (ceftriaxone, cefotaxime), carbapenems, monobactams
- Glycopeptides → vancomycin
- Others → bacitracin
2. Disruptors of the Cell Membrane
Mechanism: The mechanism involves the use of bactericidal compounds to disrupt the bacterial cell membrane, which increases permeability and results in the release of essential intracellular components.
Examples:
- Polymyxins (effective against Gram-negative bacteria)
- Gramicidin, Tyrocidine (Gram-positive bacteria)
3. Protein Synthesis Inhibitors
Mechanism: By targeting the bacterial 30S or 50S ribosomal subunits, these might be either bactericidal or bacteriostatic.
Examples:
- 50S inhibitors → erythromycin (macrolide), chloramphenicol, linezolid (oxazolidinone)
- 30S inhibitors → tetracyclines, streptomycin, gentamicin, amikacin
4. Inhibitors of Nucleic Acid Synthesis
Mechanism: Killing bacteria with substances that disrupt DNA transcription or replication.
Examples:
- DNA inhibitors → nalidixic acid, ciprofloxacin, norfloxacin, novobiocin
- RNA inhibitors → rifampicin
5. Folate Pathway Inhibitors (Antimetabolites)
Mechanism: These substances are bacteriostatic, preventing vital enzymes in the folic acid pathway that are necessary for the production of DNA and RNA.
Example:
- Sulfonamides: Prevents the conversion of PABA to dihydrofolic acid.
- Trimethoprim: Blocks the conversion of dihydrofolate reductase (DHF) to tetrahydrofolate (THF).
Applications of Antibiotics
1. Antibiotics that kill tumors
Some antibiotics, like actinomycin D and mitomycin C, are used as chemotherapeutic agents due to their ability to damage DNA in rapidly dividing cancer cells.
2. In Human Medicine
Antibiotics revolutionized healthcare by treating diseases such as pneumonia, tuberculosis, syphilis, meningitis, and sepsis.
3. Antibiotics that preserve food
- The canning industry uses some antibiotics (such as chlortetracycline), while the preservation of fish, meat, and poultry makes use of others (such as Pimaricin nisin).
- Governments typically regulate the use of antibiotics in food preservation.
4. Uses of antibiotics in veterinary medicine and animal feed
- Up until a while ago, antibiotics (penicillins, tetracyclines, erythromycins) were used extensively in the production of animal feeds. Due to this indiscriminate usage, antibiotic resistance has emerged in both humans and animals.
- A new class of antibiotics, such enduracidin and tylosin, have been created for use in animal feed.
- In a similar vein, some antibiotics, such as hygromycin B, theostrepton, and salinomycin, have been created for use only in veterinary medicine.
5. Using antibiotics to manage plant diseases
Several antibiotics have been created in recent years for the sole purpose of treating plant diseases, such as blasticidin, tetranactin, and polyoxin.
6. The Use of Antibiotics as Tools in Molecular Biology
- At the molecular level, some antibiotics are able to target particular biological processes.
- In reality, these antibiotics are useful instruments for learning about the life sciences.
- As a result, a few key details about DNA replication, transcription, and translation have been gleaned from the usage of particular antibiotics.
Examples of Main Antibiotics
- Penicillins → Penicillin G, Amoxicillin, Ampicillin
- Cephalosporins → Cefalexin, Ceftriaxone, Cefepime
- Carbapenems → Imipenem, Meropenem
- Monobactams → Aztreonam
- Glycopeptides → Vancomycin, Teicoplanin
- Aminoglycosides → Streptomycin, Gentamicin, Amikacin
- Tetracyclines → Doxycycline, Minocycline
- Macrolides → Erythromycin, Azithromycin
- Chloramphenicol → Chloramphenicol
- Lincosamides → Clindamycin
- Fluoroquinolones → Ciprofloxacin, Levofloxacin
- Rifamycins → Rifampicin
- Sulfonamides & Trimethoprim → Co-trimoxazole
- Polypeptides → Polymyxin B, Colistin
Sources of Antibiotics
Antibiotics are natural, semisynthetic, or synthetic compounds that inhibit or kill bacteria. Their sources can be grouped into three main categories:
- Microbial Sources (Natural Antibiotics)
- Semisynthetic Antibiotics
- Synthetic Antibiotics
1. Microbial Sources (Natural Antibiotics)
Many antibiotics are produced by microorganisms as part of their survival strategy to outcompete other microbes.
a) Bacteria
Actinomycetes (especially Streptomyces) → Produce more than 60% of known antibiotics.
- Streptomyces griseus → Streptomycin
- Streptomyces venezuelae → Chloramphenicol
- Streptomyces aureofaciens → Tetracyclines
Bacillus species
- Bacillus subtilis → Bacitracin
- Bacillus polymyxa → Polymyxins
b) Fungi
Penicillium notatum → Penicillin
Cephalosporium acremonium → Cephalosporins
2. Semisynthetic Antibiotics
Derived by chemically modifying natural antibiotics to improve stability, spectrum, or resistance to bacterial enzymes.
Examples:
- Amoxicillin & Ampicillin (from Penicillin G)
- Methicillin (penicillin derivative resistant to penicillinase)
- Cephalexin (from cephalosporins)
3. Synthetic Antibiotics
Entirely manufactured in laboratories using chemical synthesis, not produced by microbes.
Examples:
- Sulfonamides
- Fluoroquinolones (Ciprofloxacin, Norfloxacin)
- Oxazolidinones (Linezolid)
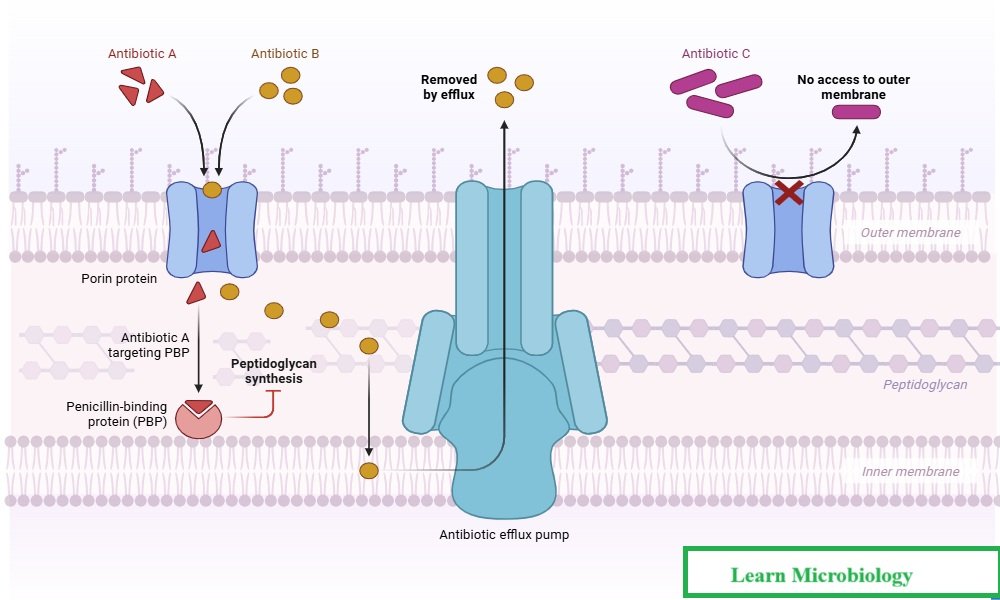
Antibiotic Resistance: A Global Threat
While antibiotics save millions of lives, misuse and overuse have accelerated the rise of antimicrobial resistance (AMR). Resistant strains such as MRSA (Methicillin-resistant Staphylococcus aureus) and multidrug-resistant tuberculosis (MDR-TB) highlight the urgent need for responsible antibiotic use.
Strategies to combat resistance include:
- Limiting unnecessary prescriptions.
- Completing full treatment courses.
- Developing new antibiotics and alternatives (phage therapy, antimicrobial peptides, CRISPR-based antimicrobials).
Frequently Asked Questions (FAQ)
Q1. What are antibiotics?
Antibiotics are medications used to treat bacterial infections by killing bacteria or inhibiting their growth. They are ineffective against viral infections.
Q2. Who discovered antibiotics?
Alexander Fleming discovered penicillin in 1928, later developed into medicine by Florey, Chain, and Heatley.
Q3. How do antibiotics work?
Antibiotics function by targeting specific bacterial processes or structures, such as cell wall synthesis or protein production, thereby disrupting the bacteria's ability to survive and reproduce.
Q4. What are the common side effects of antibiotics?
Common side effects of antibiotics may include nausea, diarrhea, vomiting, and allergic reactions. It's important to consult a healthcare provider if side effects are severe or persistent.
Q5. Can antibiotics be used to treat viral infections?
No, antibiotics are not effective against viral infections such as the common cold or flu. Antiviral medications are required for treating viral illnesses.
Q6. Why is it important to complete a prescribed course of antibiotics?
Completing a prescribed course of antibiotics is crucial to ensure all bacteria are eliminated, reducing the risk of developing antibiotic resistance and preventing the infection from returning.
Q7. What should I do if I miss a dose of antibiotics?
If you miss a dose of antibiotics, take it as soon as you remember. If it's close to the time of your next dose, skip the missed dose and continue with your regular schedule. Do not double the dose.
Conclusion
Since the invention of penicillin, antibiotics have revolutionized medicine by providing effective treatment for bacterial infections and saving millions of lives. Their mechanisms of action are varied, including interfering with metabolic routes, blocking protein or nucleic acid production, and disrupting cell walls.
In addition to human health, antibiotics have uses in molecular biology, agriculture, food preservation, and veterinary medicine. Antibiotic misuse and overuse, on the other hand, have resulted in the development of antibiotic resistance, which poses a significant threat to public health worldwide.
As a result, even if antibiotics are still one of the most significant medical advances, their sensible and prudent use is necessary to maintain their efficacy for future generations.
Also Read
- HIV and AIDS: Structure, Transmission, Symptoms, Diagnosis and Prevention
- Detection of Viruses: Modern Methods, Applications, and Advancements
- Single Cell Protein (SCP): Sources, Production, Advantages, Disadvantages & Applications
- Molecular Blotting: Techniques, Uses, and Significance
- Microbiology: From Microorganisms to Career Opportunities
- Immune System Cells: The Body’s Cellular Defenders
- Medical Microbiology Quiz
- Basic Microbiology Quiz
- Microbiology Notes
Reference and Sources
- https://www.sciencenewstoday.org/what-is-an-antibiotic-definition-types-uses-how-theywork
- https://medical-news.org/the-concerning-truth
- https://www.biologydiscussion.com/antibiotics/
- www.sciencenewstoday.org/what-is-an-antibiotic-definition-types-uses-how-they-work
- www.theportlandclinic.com/antibiotics-side-effects-and-strategies/
- https://pmc.ncbi.nlm.nih.gov/articles
- https://www.healthline.com/health/missed-antibiotic-dose
- clinicalsci.info/antimicrobial-mechanism-of-action/
- https://www.britannica.com/science/antibiotic
- https://www.msdmanuals.com/…/overview-of-antibiotics
- bing.com/videos
- https://biologyinsights.com/folate-synthesis
- pharmacyfreak.com/mechanism-of-action-of-sulfonamides/
- https://iloveveterinary.com/blog/animal

